New Cancer Screening Guideline Calls For Less and More Simplification

An updated cervical cancer screening guideline from the American Cancer Society reflects the rapidly changing landscape of cervical cancer prevention in the USA.
Published on July 30, 2020, the new guideline calls for less and more simplified screening.
And, recommends that women initiate cervical cancer screening at age 25 and that primary human papillomavirus (HPV) testing (HPV testing without the Pap test) every 5 years be the preferred method of testing through age 65.
The guideline says using HPV testing in combination with a Pap test (called co-testing) every 5 years or Pap tests alone every 3 years are acceptable options for now, as not all labs have transitioned to primary HPV testing.
The previous ACS guideline, released in 2012, called for screening starting at age 21. Since then, HPV vaccination rates have improved in the USA.
“These streamlined recommendations can improve compliance and reduce potential harms,” said Debbie Saslow Ph.D., managing director, HPV & GYN Cancers for the American Cancer Society, in a press statement.
“They are made possible by some important developments that have allowed us to transform our approach to cervical cancer screening, primarily a new understanding of the role of HPV and the development of tools to address it.”
HPV is the cause of nearly all cervical cancers.
Evidence shows the HPV test is more accurate than the Pap test and can be done less often; one HPV test every five years is more effective than a Pap test every three years, and even every year as was recommended in the 1980s and 1990s, in reducing the risk of cervical cancer.
A negative HPV test is linked to a very low cervical cancer risk. In addition, a vaccine for HPV has been in use for nearly 15 years, and more women of screening age are now vaccinated and protected from the majority of cervical cancers.
Data suggest HPV vaccination has led to a drop in rates of precancerous cervical changes, the precursors to cancer. In addition, cervical cancer incidence is low in this age group.
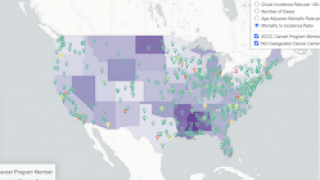
Cancer registry data from 2011 to 2015 indicates an estimated 108 cases of invasive cervical cancer in women 20 to 24 years in the U.S. each year. There are also potential harms related to the treatment of precancerous cells identified by screening including preterm birth; and screening has not been shown to lower the rate of cancer in women in this age group.
Also, most HPV infections in women in this age group become undetectable in 1-2 years. Those factors led the ACS to move the recommended age to initiate cervical cancer screening to 25.
“We estimate that compared with the currently recommended strategy of cytology (Pap testing) alone beginning at age 21 and switching to co-testing at age 30 years, starting with primary HPV testing at age 25 prevented 13% more cervical cancers and 7% more cervical cancer deaths,” said Dr. Saslow.
“Our model showed we could do that with a 9% increase in follow-up procedures, but with 45% fewer tests required overall.”
American Cancer Society screening guidelines are created by the Guideline Development Group (GDG), with 11 clinicians and population health care professionals, and a patient advocate appointed by the ACS Board of Directors to create all of its cancer screening guidelines.
To avoid professional conflicts of interest, the GDG considers content specific input and the opinions of expert clinical specialists but is responsible for supervising the review of the evidence and transforming the evidence into writing the guidelines.
Vax-Before-Cancer publishes HPV testing news.
Our Trust Standards: Medical Advisory Committee