Does Religion Influence Cervical Cancer Rates?

A new study conducted at the University of South Florida (USF) found religion and spiritual beliefs may be contributing factors in explaining why many female college students have not been inoculated to prevent cervical cancer.
This study published online in the Journal of Religion and Health on July 27, 2019, found 25 percent of female college students had not been vaccinated for human papillomavirus (HPV), and sexual activity was the main factor related to vaccination decisions.
Of those unvaccinated students in this study, 70 percent identified with a particular religious faith that promotes sexual abstinence until marriage.
But, despite their religious identification, a majority of the 307 students surveyed by USF say ‘they are sexually active.’
“The whole point of the (HPV) vaccine is to protect people against high-risk types of HPV before exposure – before they’re sexually active,” said lead author Alicia Best, Ph.D., assistant professor in the USF College of Public Health.
“So, while a student’s parents may have previously opposed the HPV vaccine for religious or other reasons, these college students may make a different decision now,” said Dr. Best in a press release.
These USF researchers concluded ‘health promotion efforts should highlight the importance of HPV vaccination regardless of current sexual activity and may benefit from partnerships with religious/spiritual organizations.’
The most reliable way to avoid transmission of sexually transmitted diseases, including HPV, is to abstain from sexual activity, says the Centers for Disease Control and Prevention (CDC).
Latex condoms, when used consistently and correctly, are highly effective in preventing the sexual transmission of the HPV virus.
While there is currently no cure for the HPV virus, it is usually harmless and goes away by itself.
HPV vaccine news
Which HPV Vaccination Schedule is Best: 1, 2 or 3 Doses?
Bottom Line: HPV Vaccinations Reduce Cancer Cases
But, certain types of HPV can cause cervical cancer. Each year, HPV causes about 33,700 cases of cancers.
While HPV causes nearly all cervical cancers it is also the cause of many other cancers, including cancers of the vagina, vulva, penis, anus, rectum, and oropharynx says the CDC.
Cervical cancer can be prevented with vaccination or if found early through regular screening and follow-up treatment, such as the following:
- The Pap test (or Pap smear) looks for precancers (cell changes on the cervix that might become cervical cancer if they are not treated appropriately).
- HPV tests look for the virus that can cause cell changes.
- If your doctor finds any abnormal results from a cervical cancer screening test, make sure to follow up in case you need treatment or further tests.
The Gardasil 9 vaccine works best if vaccination is complete well before they start having sex — and being realistic, not only is it hard to predict exactly when that will happen but once teens get older it’s not always as easy to be sure they go to the doctor and get vaccinated.
Gardasil 9 consists of HPV proteins, Types 6, 11, 16, 18, 31, 33, 45, 52, and 58, amorphous aluminum hydroxyphosphate sulfate, yeast protein, sodium chloride, L-histidine, Polysorbate 80, sodium borate, and water for injection.
HPV vaccination rates are increasing. In 2017, 66 percent of adolescents ages 13-17 years received the 1st HPV vaccine dose. On average, the percentage of adolescents who started the HPV vaccine series increased by 5 percentage points each year over the past five years (2013-2017).
However, 51 percent of these adolescents had not completed the HPV vaccine series.
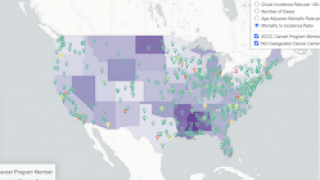
Another HPV vaccination influencer is location.
The CDC says the number of adolescents who received the 1st dose of the HPV vaccine was 11 percentage points lower in rural areas when compared to urban areas.
The vast majority of vaccine side effects are mild, such as fever or muscle pain, and last only a day or two says the CDC.
Moreover, all vaccine side effects should be reported to a healthcare provider or the CDC.
This study was funded by an Interdisciplinary Research Grant from the USF College of Public Health awarded to Dr. Cheryl Vamos (co-author on the manuscript). No conflicts of interest were disclosed.
Our Trust Standards: Medical Advisory Committee
- Religion Associated with HPV Vaccination Rate for College Women
- Examining the Influence of Religious and Spiritual Beliefs on HPV Vaccine Uptake Among College Women
- Associations Between Religion-Related Factors and Cervical Cancer Screening Among Muslims in Greater Chicago
- Religion and HPV vaccine-related awareness, knowledge, and receipt among insured women aged 18-26 in Utah
- Barriers and facilitators to HPV vaccination of young women in high-income countries
- “My mom said it wasn't important”: A case for catch-up human papillomavirus vaccination among young adult women in the US
- CDC: Condom Efectiveness/Fact Sheet for Public Health Personnel