Zika is an Under-Recognized Clinical Entity

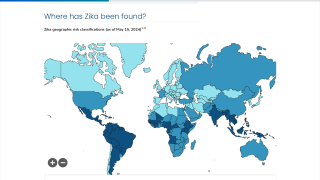
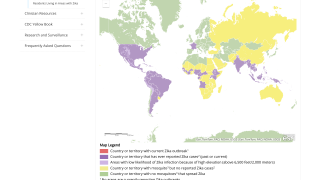
The Zika virus pandemic in the Americas and Caribbean was known to cause over 1 million cases and there were reports in which the virus was found to cause severe, life-threatening complications among patients with associated comorbidities.
From a clinical standpoint a recent study reported that until 2013, the Zika virus (ZIKV) was generally considered to cause a mild, self-limiting illness, which did not pose a serious public health threat.
However, it was not until the first non-perinatal death was identified in a 15-year-old girl from northern Colombia in October 2015, that an increasing number of ZIKV-associated fatalities were reported in the literature.
The case from Malaysia reported in the current issue of the International Journal of Infectious Diseases, confirms that ZIKV infection can result in atypical disease and lead to severe and even fatal outcomes.
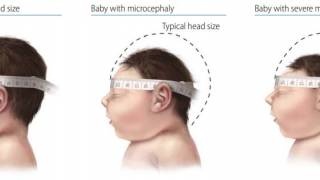
Previous to this report, the majority of fatalities associated with ZIKV infection were almost invariably linked to acute neurological complications.
However, amongst those exceptional fatalities without neurological involvement, the question was raised as to whether ZIKV could cause renal and cardiac involvement, as was observed on autopsy examinations of the case described in this issue.
Renal and cardiac complications have been reported in atypical, severe and fatal cases of chikungunya virus (CHIKV) infection.
Conversely, cases of ZIKV infection with documented renal or cardiac complications have been reported rarely and have usually lacked detailed histopathological evaluation as well as molecular confirmation of the presence of viral RNA within the renal or cardiac tissues during the routine autopsy of fatal cases.
ZIKV infection has previously been reported to cause cardiovascular compromise as a consequence of systemic infection, as revealed by electrocardiographic and echocardiographic alterations, even including venous thromboembolism (in ZIKV and CHIKV infections), as well as demonstrating myocardial inflammation secondary to viral infection.
Autopsy examinations of a heart transplant recipient who developed ZIKV infection revealed plasma cell infiltrates in the myocardial tissue, along with perivascular and endovascular damage.
Nevertheless, publications in the literature on cardiovascular manifestations in adult patients with ZIKV infection are scarce, and the case report by Rajahram et al. (2019) is timely in underscoring how this arboviral infection can produce unexpected clinical complications with renal and cardiovascular involvement.
Previous reports have suggested an association between cardiovascular complications and ZIKV during the acute phase of the infection.
However, only a limited number of studies have addressed this potential association.
Findings in patients (Abdalla et al., 2018) and non-human primates (Li et al., 2016) have provided evidence that ZIKV has a broad tissue tropism, which includes renal and heart tissues.
Nevertheless, further investigations are needed in order to delineate the underlying pathogenic processes in which ZIKV affects myocardial tissue and to characterize the spectrum of cardiovascular manifestations caused by this emerging arboviral infection.
It should be emphasized that the pathogenesis of severe ZIKV infection remains poorly understood.
In vitro and experimental animal models have provided evidence that antibody-dependent enhancement (ADE) may play a role, but clinical correlates for this phenomenon still need to be confirmed in human ZIKV infection.
Recent studies suggested that preexisting high antibody titers to the dengue virus were associated with a reduced risk of acquiring ZIKV infection and disease.
In this sense, the landscape of ZIKV immunity that now exists may affect the risks of future transmission.
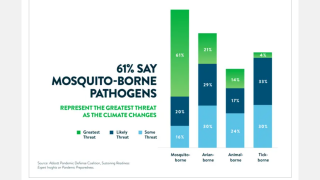
Co-circulation with other arboviruses and ADE poses a challenge for physicians and public health authorities, given the potential to confound and delay diagnosis and possibly influence poorer outcomes in patients with previous exposure to other flaviviruses.
As a result, multiple research networks on ZIKV and arboviruses, in general, have been established, which can leverage protocols, methodologies, and multidisciplinary approaches to inform treatment, prevention, and control strategies.
Although recent advances have greatly contributed to our understanding of ZIKV pathogenesis, systemic involvement and the expanding tissue tropism of this virus and its potential relationship to different lineages highlight important aspects for future investigation.
Finally, it is worth considering the setting for vaccine development and preparedness for other emerging arboviruses in Latin America and the Asia-Pacific region, such as Ross River, Mayaro, Oropouche, Madariaga, West Nile, and the Venezuelan equine encephalitis and Eastern equine encephalitis viruses.
Zika virus research news published by Zika News.
Our Trust Standards: Medical Advisory Committee