What is Paxlovid’s Absolute and Relative COVID-19 Risk Reduction

The New England Journal of Medicine (NEJM) recently published an Editorial related to understanding who benefits the most when taking the oral COVID-19 treatment Paxlovid.
Paxlovid (Nirmatrelvir, plus ritonavir) is the first oral small-molecule antiviral agent administered targeting the SARS-CoV-2 virus main protease inhibitor with potent pan–human-coronavirus activity in vitro.
The U.S. FDA and various countries have authorized Paxlovid.
Since December 2021, the U.S. government has distributed about 863,000 Paxlovid treatments in the U.S., including (175,000) during the week of Mar. 14, 2022.
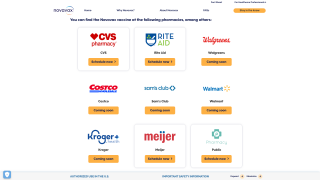
Furthermore, Paxlovid is a key component of the U.S. government’s ‘Test & Treat’ program now offered at certain pharmacies.
A recent phase 3 clinical trial funded by Pfizer Inc. found that treating symptomatic COVID-19 with Paxlovid resulted in an 89% risk reduction of progression to severe COVID-19 without evident safety concerns.
Excerpts from the Editorial are inserted below:
The study results are clear, but it is worth considering the difference between absolute and relative risk reduction.
Although the relative risk reductions were large and similar across most subgroups (at about 89%), those at lower risk had a very small absolute benefit.
For example, in patients who were SARS-CoV-2 seronegative at baseline, the absolute risk reduction was about 10% points.
However, in those who were SARS-CoV-2 seropositive at baseline, either because they had been infected in the past or had already undergone seroconversion from their current infection, the absolute risk reduction was about 1% point.
Thus, although all groups seem to have a similar relative benefit, the most significant absolute benefit is among those at the highest risk.
Furthermore, this trial was performed between mid-July and early December 2021, a period when the delta variant was most likely responsible for the majority of infections.
‘We do not yet know how Paxlovid will perform as new variants, such as omicron, emerge,’ wrote these researchers.
‘And, finally, until we have a better idea of the potential for the emergence of resistance, we need to be good stewards of this medication. By limiting its use to those most likely to benefit, we can potentially prolong its useful life,’ concluded this NEJM Editorial.
Previously, the U.S. CDC reported among 1.2 million persons who completed primary vaccination during December 2020–October 2021, severe COVID-19 associated outcomes (0.015%) or death (0.0033%) were rare.
All persons with severe outcomes had at least one risk factor and 78% of persons who died had at least four.
However, as of Mar. 17, 2022, the U.S. NIH OpenData Portal shows Nirmatrelvir as effective against various SARS-CoV-2 variants, including Omicron’s emerging sublineages, as does the European Medicines Agency.
PrecisionVaccinations publishes fact-checked research-based antibody, antiviral, and vaccine news.
Note: This news article edited study results and editorial for clarity and was curated for mobile readers.
Our Trust Standards: Medical Advisory Committee
- The Potential of Intentional Drug Development
- Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19
- EPIC-HR: Study of Oral PF-07321332/Ritonavir Compared With Placebo in Nonhospitalized High Risk Adults With COVID-19
- OpenData Portal | SARS-CoV-2 Variants & Therapeutics
- PAXLOVID Oral Antiviral (Nirmatrelvir)