Pancreatic Cancer Vaccine Concept Found Effective in Mice
A new study published by UK and China researchers created an effective vaccine development system that doubled the survival time of mice with pancreatic cancer.
Importantly, this innovative vaccine system can be personalized for each individual receiving it.
This is important news since the genetic makeup of cancer varies from individual to individual, and treatments that are effective for one patient’s cancer may not be effective against another’s.
This pre-clinical, proof-of-concept study was published on November 25, 2019, in Clinical Cancer Research, a journal of the American Association for Cancer Research.
Professor Yaohe Wang, M.D., Ph.D.,from the Queen Mary University of London and the Sino-British Research Centre at Zhengzhou University in China, who led the study, said in a related press release, “Development of a preventive vaccine against non-viral cancers is hugely limited by the lack of appropriate tumor antigens and an effective approach to induce robust anti-tumor immunity against those antigens.”
“This is preliminary data from tests on mice but it could be a platform for developing personalized and powerful prophylactic cancer vaccines to reduce pancreatic cancer incidence in at-risk individuals.”
They developed a novel individualized prophylactic and therapeutic vaccination regimen using induced pluripotent stem cells (iPSCs), gene editing and tumor-targeted replicating oncolytic viruses.
And, they created a Virus-Infected, Reprogrammed Somatic cell-derived Tumor cell (VIReST) regime.
iPSCs from healthy cells were introduced to pancreatic tumor cells using in situ gene editing via the stable provision of KRAS G12D and p53 R172H tumor driver mutations.
These cells were pre-infected with oncolytic Adenovirus (AdV) as prime or Vaccinia virus (VV) as a boost, to improve vaccine immunogenicity, prior to delivery of vaccines in a sequential regime to young transgenic mice, genetically programmed to develop pancreatic cancer, to prevent the disease development.
This study found tumor cells pre-infected with oncolytic AdV as prime or VV as a boost, was the best regime to induce tumor-specific immunity.
iPSC-derived tumor cells were highly related in antigen repertoire to pancreatic cancer cells of transgenic mice, suggesting that individuals' stem cells can provide an antigenically matched whole tumor cell vaccine.
By injecting these virus-infected cells into mice that were destined to develop pancreatic cancer, the research team was able to delay the onset of disease, doubling their survival time, when compared with mice who did not receive the vaccine.
Notably, because the cells were derived from the mice that were going to receive the vaccine, the cells created were genetically similar to cancer that was going to develop in these mice, said these researchers.
This suggests that cells could be taken from at-risk individuals and used to create matching tumor cells for use in a vaccine regime tailored to those individuals.
Pancreatic cancer has the lowest survival rate of all the common cancers. most pancreatic cancers (93%) are exocrine adenocarcinoma. In 2019, an estimated 56,770 adults in the USA will be diagnosed with pancreatic cancer, says Cancer.net.
Dr. Louisa Chard Dunmall, a senior postdoctoral research fellow at Queen Mary, added, “One reason for this low survival rate is lack of symptoms, meaning diagnosis is often not made until the cancer is at an advanced stage.”
“This suggests a window of opportunity for the application of preventative vaccine strategies.”
“Although this research is at the early developmental stages, it provides strong evidence that the creation of a vaccine against pancreatic cancer is possible,” concluded Dr. Dunmall.
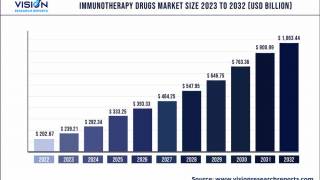
The research team will now look at different ways of improving the regime – including increasing the number of vaccinations or combining the vaccine with other therapies such as immunotherapies.
The research was undertaken by scientists from the Barts Cancer Institute at Queen Mary, the Sino-British Research Centre at Zhengzhou University and the Guangzhou Institutes of Biomedicine and Health, Chinese Academy of Sciences.
The Sino-British Research Centre is a joint venture established by Queen Mary and Zhengzhou University.
The research was funded by the Chinese Ministry of Science and Technology and Zhengzhou University. No conflicts of interest were disclosed.
Cancer Research News is published by Vax Before Cancer
Our Trust Standards: Medical Advisory Committee