San Diego Should React Faster to Disease Outbreaks

A new audit by the state of California says San Diego’s lack of urgency in responding to a 2017 hepatitis A outbreak led to 20 deaths.
San Diego County officials identified the hepatitis A outbreak in March 2017 and were able to later trace some cases back to November 2016.
San Diego public health declared an emergency on September 1, 2017, and stayed in effect until January 23, 2018.
This hepatitis A outbreak spread quickly among San Diego’s homeless population due to unsanitary conditions and was spread throughout the local population.
Hepatitis A is a communicable disease of the liver caused by the hepatitis A virus. It is usually transmitted person-to-person through the fecal-oral route or consumption of contaminated food or water, says the Centers for Disease Control and Prevention (CDC).
California State Auditor Elaine Howle released this audit on December 21, 2018, saying the region’s current plan to avoid another health emergency ‘still falls short,’ according to CourthouseNews.com.
While the California Department of Public Health worked with the city and county on changes to improve future efforts to curb the spread of disease, the auditor found these changes still lacked two critical components:
- establishing a timeframe for meeting vaccination targets, and
- determining the number of nurses or health care workers needed to get those vaccines administered within that timeframe.
Additionally, San Diego County and City ‘were slow to install hand-washing stations and increasing access to restrooms for the homeless until months after their initial discussions,’ according to the audit.
“The lack of urgency, the lack of action for months at a time may have come from the fact we’re talking about some of the most vulnerable and most ignored people in our community,” said Assemblyman Todd Gloria at a press conference.
“I think the lesson learned from this is we may choose to ignore those people, but we do it at our own peril. I hope moving forward we can act not as though those people don’t matter because they do matter – this report shows they do matter.”
“This shouldn’t happen ever again,” Gloria added.
The County of San Diego released an ‘After Action Report’ that summarizes the County’s response to this hepatitis A outbreak.
The purpose of an after action report is a self-evaluation to document an agency’s response after an emergency.
This ‘Hepatitis A Outbreak After Action Report’ looks at the County’s response to the local health emergency and actions taken during the outbreak to assess what worked well, what could be improved, and a plan for making recommended improvements.
The report also highlights several novel approaches taken to combat the outbreak including the use of foot teams. The teams paired up County Health and Human Service Agency public health nurses with homeless outreach workers and public safety officers who were deployed to provide vaccinations and education in homeless encampments, difficult to reach areas near river beds, in canyons and at locations that provide services to homeless people.
To help address one high-risk group, the CDC’s Advisory Committee on Immunization Practices approved on October 25th, 2018, the ‘recommendation for routine hepatitis A vaccination for all people experiencing homelessness.’
Since the San Diego hepatitis A outbreak was among the first of many reported around the USA during 2017 and 2018, this audit may offer insights for other states to implement.
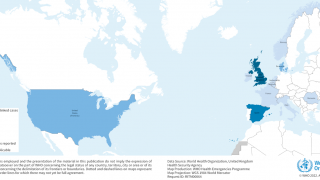
Currently, the states of Arkansas, California, Indiana, Illinois, Kentucky, Michigan, Missouri, North Carolina, Ohio, Tennessee, Utah, and West Virginia are reporting widespread hepatitis A outbreaks.
As an example, the Dallas County Health and Human Services department quickly responded to local reports and dispatched mobile clinics to homeless centers across Dallas, Texas, to administer vaccinations to help prevent and fight Hepatitis A.
And, in Lexington, Kentucky, the restaurant owners and employees fully cooperated with local health officials by closing the building, cleaning it, quarantined infected employees, and proactively communicated vaccination options with customers.
While it is relatively uncommon for restaurant customers to become infected with the hepatitis A virus due to an infected food handler, anyone who consumed food or drinks during the stated time period is advised to get a hepatitis A vaccination, says the CDC.
To request a hepatitis vaccination appointment at a local pharmacy, please visit this page.
The CDC Vaccine Price List displays current hepatitis vaccine contract prices and general information.
And, vaccine discounts can be found here.
Vaccines, like any medicine, can have side effects. You are encouraged to report negative side effects of vaccines to the FDA or CDC.
Our Trust Standards: Medical Advisory Committee
- Hepatitis A Outbreak in San Diego County is Officially Over
- San Diego Hepatitis A Outbreak 2017-18 After Action Report
- San Diego’s Hepatitis A Outbreak
- Viral Hepatitis
- Hepatitis A Outbreak in Tennessee Turns Fatal
- Florida is the Newest Hepatitis A Hot-Spot
- Hepatitis A Vaccination Now Recommended for the Homeless Population