West Nile Relocated From Nebraska to the US Southwest During 2019

As the number of West Nile virus cases and related fatalities slow down, various researchers are trying to answer ‘why did they shift to the southwest?
As of December 17, 2019, California (213), Arizona (173) and Colorado (120), Nevada (44) and New Mexico have reported a total of 590 West Nile virus ( WNV) cases during 2019.
These states represent about 64 percent of all West Nile virus (WNV) cases (910) reported by the Centers for Disease Control and Prevention (CDC) during 2019.
Of these WNV cases, 66 percent were classified by the CDC as a Neuroinvasive Disease, such as meningitis or encephalitis.
And, according to the Arizona Department of Health, there have been 18 WNV related fatalities confirmed this year. This indicates Arizona has reported 36 percent of all WNV deaths (49) in the USA during 2019.
The good news from this new data is that 2019 is coming to a close reporting far few WNV cases and fatalities when compared with 2018.
During 2018, the CDC confirmed 2,647 WNV cases and 167 related fatalities.
Furthermore, the state of Nebraska was the unfortunate 2018 WNV leader, confirming 251 cases and 11 fatalities.
To learn why the volume of WNV cases shifted to the southwest, various researchers conducted real-world studies.
As an example, after sequencing more than 400 different genomes of the West Nile Virus, a Northern Arizona University (NAU) scientist discovered ‘local cases came from 2 different places.’
One WNV case migrated from the Phoenix, Arizona area. The other case is a bit more of a mystery.
Evolutionary biologist Crystal Hepp, Ph.D., with NAU, is a leader in the effort to better understand how the West Nile Virus circulates in the American Southwest, and said in a press release issued on September 13, 2019, “We often think the simplest answer is the most likely answer.”
Dr. Hepp recently received a New Investigator Award grant from the Arizona Department of Health Services, for a project to investigate the circulation and source locations of the WNV.
“It would have made sense if these two strains, separated by only 10 miles, were due to the same importation event.”
“From a public health perspective, finding that these two strains are from two different places is good news.”
“If they were closely related, it would mean that WNV had likely been cycled through birds and mosquitoes across 10 miles of Coconino County.”
“WNV from Maricopa County has spilled over into Washington County, Utah; Riverside County, California; and Yuma County, Arizona in the past, and we would like to move forward with a predictive model that could inform counties of risk based on historical patterns and environmental data, concluded Dr. Hepp.
West Nile virus news
- West Nile Virus Primarily Confirmed In Western States
- West Nile Neuroinvasive Cases Increased 25% in 2018
- 3 Human Cases of West Nile Virus Confirmed in Texas
Further to the west, when the California WNV outbreak began to accelerate in June 2019, the California Department of Public Health (CDPH) issued a statement urging everyone to protect themselves from mosquito bites during the WNV season, which usually extends through early fall.
"West Nile virus activity in the state is increasing, so it is important to take every possible precaution to protect against mosquito bites," said State Public Health Officer and CDPH Director Dr. Karen Smith, in this press release.
According to CDPH, prevention is key, since there are no vaccines to prevent or medications to treat WNV in people.
The Centers for Disease Control and Prevention (CDC) says ‘it's unclear what factors have led to the geographical shifts in WNV cases in 2019, especially considering West Nile virus outbreaks are generally related to rainy Spring and Summer seasons.
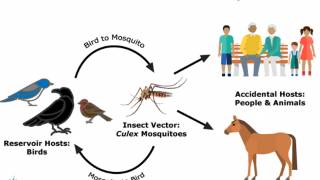
Historically, the WNV transmission cycle is influenced by weather conditions and exists in areas where the virus infects birds, humans, horses, and other mammals.
The West Nile virus usually circulates between Culex sp. mosquitoes, and birds. A mosquito feeds on an infected bird, acquires the WNV, then passes the virus to humans, who are considered ‘dead-end’ hosts, as they cannot pass the WNV on to other humans.
Among other drivers, weather conditions have direct and indirect influences on vector competence, on the vector population dynamic and on the virus replication rate within the mosquito, which are mostly weather dependent.
Most people (80%) infected with West Nile virus do not develop any symptoms, says the CDC.
Serologically, WNV is a member of the Japanese encephalitis serocomplex. The viruses can be designated into at least 5 phylogenetic lineages, but only lineages 1 and 2 have been associated with significant disease outbreaks in humans.
This leads the CDC to suggest ‘healthcare providers should consider arboviral infections in patients with aseptic meningitis or encephalitis, and perform diagnostic testing as appropriate.’
West Nile virus is a single-stranded ribonucleic acid (RNA) virus. It is a member of the Flavivirus family, which also contains Zika virus, dengue virus and yellow fever virus.
Laboratory diagnosis of WNV is generally accomplished by testing serum or cerebrospinal fluid to detect WNV-specific IgM antibodies
> West Nile Virus Testing Service at UltaLabs <
Although a number of preclinical vaccine approaches have been developed, for West Nile, few have proceeded to human clinical trials.
There is one WNV vaccine candidate, HydroVax-001, conducting a small, early-stage, phase 1 clinical trial. A recent study concluded says ‘the HydroVax-001 WNV vaccine was found to be modestly immunogenic and well-tolerated at all dose levels.’
Which means, HydroVax-001 appears to be several years away from commercialization.
This means it is best to avoid mosquito bites by using insect repellent and wearing long-sleeved shirts and long pants to prevent a WNV infection in 2020.
West Nile virus news published by Precision Vaccination.
Our Trust Standards: Medical Advisory Committee
- WEST NILE VIRUS
- Latest West Nile Virus Activity in California
- Biologist: Two samples of West Nile in Coconino County came from different sources
- Increasing West Nile Virus Activity in California
- CDC: West Nile Virus Disease Cases and Presumptive Viremic Blood Donors by State – United States, 2019 (as of December 17, 2019
- CDC Disease Maps: West Nile Virus
- West Nile virus vaccines – current situation and future directions