Building Better Flu Shots Based on Antibody Responses and Genetics

A vaccine that combines antigens from different flu strains could trigger a more protective immune response than a traditional influenza vaccine, wrote the U.S. National Institute of Health (NIH).
Published on January 14, 2025, the NIH says findings from a recent study indicate a new method could enhance the effectiveness of annual flu shots.
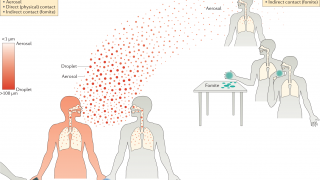
The NIH explained seasonal flu shots contain hemagglutinin (HA) molecules from various viral strains. But even when the strains in the vaccine exactly match those in circulation, the vaccines have limited efficacy.
This is because most vaccinated people produce antibodies against only one of the vaccine strains.
This "subtype bias" has two plausible explanations.
One is that prior exposure to a particular flu strain primes the immune system to respond to that strain later. Another is that variation in people's genes for key immune system components affects the vaccine response.
A research team led by Dr. Mark Davis at Stanford University School of Medicine examined the relative contributions of these mechanisms to flu vaccine responses. They aimed to use this information to develop a vaccine, limiting the biased response.
Their results, partly funded by NIH, appeared in Science on December 20, 2024.
The Editor's Summary says, 'Mallajosyula et al. gathered data from monozygotic twins and vaccinated newborns and found that biased antibody responses toward particular influenza strains found within a vaccine were more strongly linked to genetics.'
'In mouse models and a human organoid system, delivering antigens from four distinct influenza strains in a format in which they were coupled together through a scaffold increased the production of antibodies toward each strain.'
'Broader responses were correlated with increased diversity of helper T cells that support B cells in making antibodies.'
This conclusion suggests 'that coupling of heterologous antigens improves antibody responses across influenza strains by broadening T cell help... using this approach substantially improved the antibody response to avian influenza.'
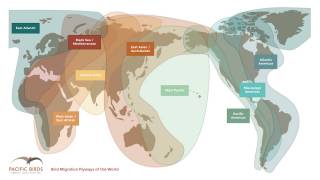
"Overcoming subtype bias this way can lead to a much more effective influenza vaccine, extending even to strains responsible for bird flu," Dr. Davis stated.
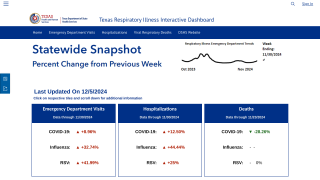
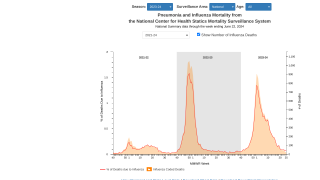
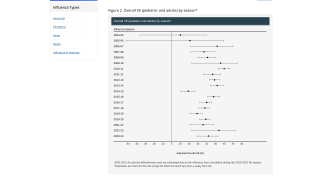
A meta-analysis of flu vaccine effectiveness (VE) studies from 2017 through 2022, published in the journal Vaccines on February 28, 2024, showed that the real-world effectiveness of seasonal influenza vaccination averaged 41.4%. The flu shot VE varied substantially by virus type and age group.
In August 2024, the U.S. CDC updated its 'Past Seasons' VE Estimates' chart.
As of January 2025, physicians, nurses, and pharmacists can offer patients up to nine influenza vaccines for the 2024-2025 flu season.
Our Trust Standards: Medical Advisory Committee