New Rabies Cases Reported in Arizona

A series of animal attacks in Arizona has state officials on alert for rabies.
On Monday, Jan. 15, 2018 a woman was bitten by a coyote on the west side of Tucson, Arizona.
"A woman on a work break resting inside her car with the passenger side door open was bit on her thigh by a coyote," reported Tucson News.
"The wound was minor, but rabies treatment was required."
According to Mark Hart, the Public Information Officer for the Arizona Game and Fish Department (AGFD), the coyote was found on January 17, near the Pima Community College community campus, and was humanely euthanized.
In another attack on Saturday, January 13, 2018, in Green Canyon, which is east of Tucson, a coyote charged a bowhunter and was later tested positive for rabies.
The good news is the hunter was not bitten.
According to Hart, “A hunter just down from a tree stand was charged by a coyote with teeth bared,” he told the Range News. “He struck it with his bow to fend off the attack, then shot the coyote with an arrow when it was down.”
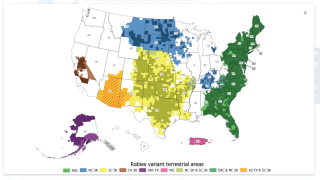
Additionally, the rabies activity in Arizona’s gray fox populations has quadrupled in the last year, according to data released by the Arizona Department of Health Services. There are 24 rabid foxes in 2017, compared with 6 rabid foxes reported statewide in 2016.
“We want to remind people to keep their dogs leashed, vaccinate pets if they’re overdue, don’t feed or approach wild animals,” said Graham Briggs, manager of the Infectious Diseases & Epidemiology department at Pinal County Public Health.
The rabies virus attacks the central nervous system, eventually causing disease in the brain and death. Death usually occurs within days of the appearance of symptoms, which may not appear for a month following a bite from a rabid animal, says the Centers for Disease Control and Prevention (CDC).
For people who have never been vaccinated against rabies previously, post-exposure anti-rabies vaccination should always include administration of both passive antibody and vaccine.
People cannot transmit rabies to other people unless they themselves are sick with rabies, says the CDC.
If people are treated within two or three days after being bitten, the human rabies vaccine is highly effective, and victims usually survive.
The estimated public health expenditures on rabies disease diagnostics, prevention, and control in the US is $245 to $510 million annually. Although the cost varies, a course of rabies immune globulin and four doses of vaccine given over a two-week period typically exceeds $3,000, reports the CDC.
Over the last 100 years, rabies in the United States has changed dramatically. The number of rabies-related human deaths in the United States has declined to one or two per year. Cats, dogs, and livestock can also become infected with rabies if they are bitten by rabid wild animals and they have not been vaccinated.
This is because modern day prophylaxis has proven nearly 100% successful, reports the CDC.
The actual number of PEP treatments given in the United States each year is unknown. However, it is estimated by the CDC to be about 40,000 cases.
There are two pre-exposure rabies vaccines approved in the USA:
- Human Diploid Cell Vaccine (HDCV): IMOVAX® RABIES (Sanofi Pasteur)
- Purified Chick Embryo Cell Vaccine (PCEC): RabAvert (GSK)
Rabies virus belongs to the order Mononegavirales, viruses with a nonsegmented, negative-stranded RNA genomes. Within this group, viruses with a distinct “bullet” shape are classified in the Rhabdoviridae family, which includes at least three genera of animal viruses, Lyssavirus, Ephemerovirus, and Vesiculovirus.
A person who is exposed and has never been vaccinated against rabies should get four doses of rabies vaccine, one dose right away, and additional doses on the third, seventh and fourteenth days.
They should also get another shot called Rabies Immune Globulin at the same time as the first dose, says the CDC.
This is because HRIG can partially suppress the active production of antibody.
The Human Rabies Immune Globulin:
- KEDRAB is a new human rabies immune globulin product in the United States approved by FDA in August 2017.
The greatest source of rabies in humans in the USA is from wild carnivores and bats. 300-400 pet dogs and cats are infected each year reports the National Center for Emerging and Zoonotic Infectious Diseases.
Around the world, rabies in dogs is still a serious health problem.
At risk, countries include most of Europe, Japan, Canada, Australia, and India.
Every year in India, 20,000 people are estimated to die from rabies. Most of the victims are children. Nearly all of the deaths occur after victims are bitten by rabid dogs.
If you are traveling to one of the at risk countries, the CDC has specific recommendations based on:
- the occurrence of animal rabies in the country of destination
- the availability of antirabies biologics
- the intended activities of the traveler, especially in remote areas
- and the traveler’s duration of stay.
For detailed information visit the CDC site.
Our Trust Standards: Medical Advisory Committee
- UPDATE: Coyote who bit woman was found, euthanized
- Coyote that charged hunter in the Chiricahuas had rabies
- Rabies Confirmed in Animals Found in Superstition Mountain Area
- Arizona Fish and Game
- Rabies VIS
- Rabies Risk Areas
- Rabies in the U.S. and around the World
- Use of a Reduced (4-Dose) Vaccine Schedule for Postexposure Prophylaxis to Prevent Human Rabie
- The Rabies Virus
- The Burden of Rabies
- Pinal County